Hospital at night, a survey of the junior orthopaedic doctor’s perspective
U Butt, R Wharton and G C Bannister
Cite this article as: BJMP 2009:2(4) 49-50
|
Introduction: The aim of the NHS Modernisation Agency’s Hospital at night project is to “Redefine how medical cover is provided in hospitals during the out of hours period.”(1) The project “requires a move from cover requirements defined by professional demarcation and grade, to cover defined by competency in order to release significant amounts of medical staff time and support the compliance with WTD (Working Time Directive) while enhancing clinical practice and training.”(1) Chairman of the BMA’s Junior Doctors Committee and also medical advisor to the Hospital at Night Project undertook a survey of junior doctors’ activity in the evening, night, and weekends. They noted that the evenings were very busy and the nights quieter, that general physicians work harder at night than those in other specialties or orthopaedic surgeons. In summary their survey showed that a huge amount of doctors’ time was wasted on tasks which did not require their level of skills. Such tasks included phlebotomy, searching for notes, and x-rays.(1) An evaluation report into the implementation and impact of the hospital at night pilot project, August 2005, identified key elements to minimize medical workload at night. These included working within a multidisciplinary, competency-based team, with extended skills ward staff to minimize reliance on the night team, reduce duplication, take away inappropriate tasks, bleep-filtering and better use of new technologies such as digital imaging and e-prescribing (2). Our aim was to assess the experience of a typical junior orthopaedic doctor’s experience during his on-call to assess their perspective of the implementation of hospital at nightand to establish whether the recommendations of the evaluation report were being implemented. Methods: A prospective review was conducted of the night duties of all junior doctors working or cross-covering trauma and orthopaedics across Frenchay and Southmead hospital sites of the North Bristol NHS Trust between December 2007 and January 2008.A questionnaire included nature of activity and level of experience, closed questions relating to the hand-over experience. Details of calls received and the nature of tasks undertaken during on-call period with times. Data were then stored and analysed using excel-office 2002. Results: Total of 51 questionnaires were completed by the junior orthopaedic doctors during their respective on-call duties. A total of 109 calls were received or tasks requested. The average time spent during hand-over was 14.1 minutes (range 5-20 minutes). Discussion: Our data indicates busiest times occurred between 21:00 – 23:00 (Fig 1) 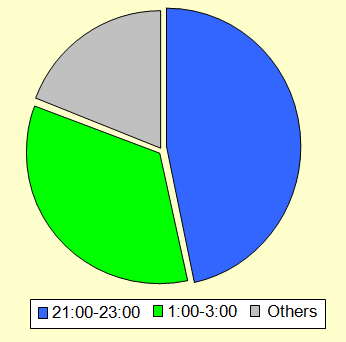 Figure 1, illustrates a distribution of the peak work-load period which occurred between 9pm-11pm and 1am-3am. This finding contradicts previous surveys done prior to the implementation of the hospital at night where it was noted that the nights were quieter and sub-specialist such as orthopaedic surgeons were not working as hard as general medics (1).
Figure 1, illustrates a distribution of the peak work-load period which occurred between 9pm-11pm and 1am-3am. This finding contradicts previous surveys done prior to the implementation of the hospital at night where it was noted that the nights were quieter and sub-specialist such as orthopaedic surgeons were not working as hard as general medics (1). 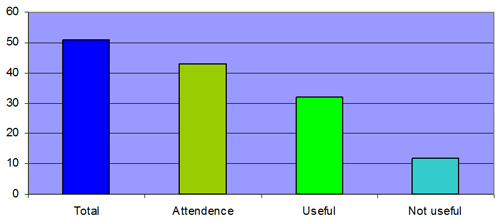 Figure 2, shows the overall experience of the hand-over as judged by the orthopaedic juniors. There was an eighty-five percent (43/51) attendance by the on-call orthopaedic juniors of which seventy-two percent (32/44) thought that it was a useful experience
Figure 2, shows the overall experience of the hand-over as judged by the orthopaedic juniors. There was an eighty-five percent (43/51) attendance by the on-call orthopaedic juniors of which seventy-two percent (32/44) thought that it was a useful experience 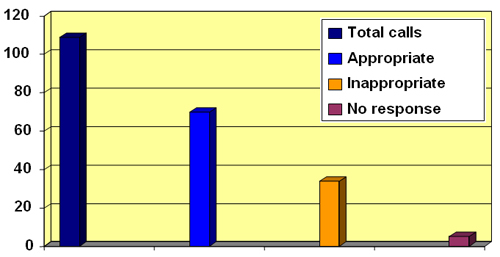 Figure 3 illustrates a distribution of the calls received. As illustrated, 37/109 calls were viewed as inappropriate The majority of the orthopaedic juniors surveyed framed hospital-at-night hand-over was useful but thirty-four percent (37/109) of the calls they received were viewed as inappropriate (Fig 2,3). The most frequent of the inappropriate ward calls were ‘requests to rewrite drug-charts’ (Fig 4,5).
Figure 3 illustrates a distribution of the calls received. As illustrated, 37/109 calls were viewed as inappropriate The majority of the orthopaedic juniors surveyed framed hospital-at-night hand-over was useful but thirty-four percent (37/109) of the calls they received were viewed as inappropriate (Fig 2,3). The most frequent of the inappropriate ward calls were ‘requests to rewrite drug-charts’ (Fig 4,5). 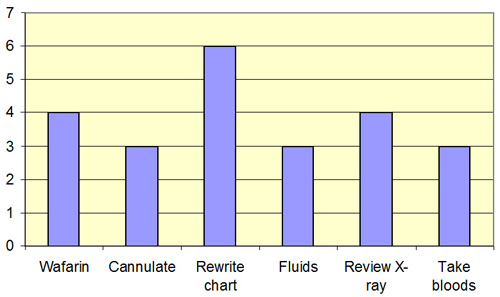 Figure 4 describes the frequencies of these calls. As illustrated the most frequently inappropriate ward-call was to ‘rewrite drug-charts’. There were twenty-three (23/37) inappropriate ward-calls
Figure 4 describes the frequencies of these calls. As illustrated the most frequently inappropriate ward-call was to ‘rewrite drug-charts’. There were twenty-three (23/37) inappropriate ward-calls 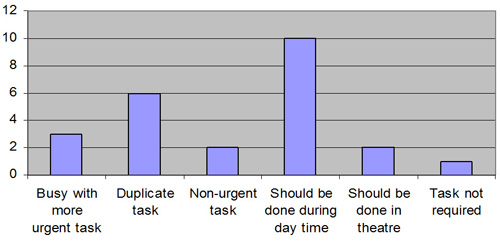 Figure 5 shows the reasons given by the on-call doctors for the inappropriate tasks. The most frequently given reason was that ‘the request should have been done during the day’. The second most frequently given reason for inappropriate calls was the fact that ‘it was a duplicated request’ Our survey also highlighted that the most frequently given reason for inappropriate tasks was firstly that the request should have been done during the day and secondly that it was a duplicated request. These findings seem to defeat the key purpose of the hospital-at-night project for an orthopaedic SHO on-call. Conclusion: Hospital at night cannot function in isolation. There are fewer doctors available then normally and the system has to use their time effectively. 30% of inappropriate calls to wards were to rewrite drug charts and to prescribe warfarin. This should have been identified and performed by the day staff. 10% of calls were to review X-rays. Much of the inappropriate activity could be pre-empted if both day and night staff attended the handover and the tasks outstanding from the day identified. The doctor on the night could then perform an hourly ward round completing these tasks without interrupting at the beginning of the night.
Figure 5 shows the reasons given by the on-call doctors for the inappropriate tasks. The most frequently given reason was that ‘the request should have been done during the day’. The second most frequently given reason for inappropriate calls was the fact that ‘it was a duplicated request’ Our survey also highlighted that the most frequently given reason for inappropriate tasks was firstly that the request should have been done during the day and secondly that it was a duplicated request. These findings seem to defeat the key purpose of the hospital-at-night project for an orthopaedic SHO on-call. Conclusion: Hospital at night cannot function in isolation. There are fewer doctors available then normally and the system has to use their time effectively. 30% of inappropriate calls to wards were to rewrite drug charts and to prescribe warfarin. This should have been identified and performed by the day staff. 10% of calls were to review X-rays. Much of the inappropriate activity could be pre-empted if both day and night staff attended the handover and the tasks outstanding from the day identified. The doctor on the night could then perform an hourly ward round completing these tasks without interrupting at the beginning of the night.
|
Author Details U BUTT, StR, Avon orthopaedic centre Southmead Hospital, Bristol, UK R WHARTON, StR, Avon orthopaedic centre Southmead Hospital, Bristol, UK G C BANNISTER, Consultant orthopaedic surgeon, Avon Orthopaedic Centre, Southmead Hospital, Bristol, UK CORRESPONDENCE: U BUTT, Bunglow 3, Frenchay Hospital , Bristol, UK. BS16 1LE. Email: doc_online74@hotmail.com |
References
- News Feature. The Hospital at Night. “Rhoda MacDonald asks Simon Eccles, chairman of the BMA’s Junior Doctors Committee and medical advisor on this project, what it is all about.” BMJ Career Focus 2004;328:19;doi;10.1136/bmj.328.7431.s19.
- “The implementation and impact of Hospital at Night pilot projects. An evaluation report”. August 2005; DOH.

The above article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.




